This is a guest post for One Nucleus by Toby Beresford. Toby is the Founder and CEO of success tracking network Rise.global. Previously he has worked as a developer of web based disease management for patients, dermatology tele-referrals for GPs and was deputy chairman of the public health sub-committee for Wandsworth Council. His email address is toby@rise.global
At the recent PRISM Series Dave Snowden told the story of how he self-managed his recovery from Type 2 diabetes – he called it his hero’s journey. It’s a story he has told before in a blog post “Early Detection, Fast Recovery”. Critically, he caught the disease early, refused to countenance “palliative” care and instead took control over his cure, targeting key factors such as diet and exercise. After 7 months he was rewarded with an all-clear diagnosis, saving himself from early death and the NHS from another expensive chronic patient.
Dave “self-optimised” to cure himself. He tracked his progress over time on key metrics and little by little he continuously improved his health.
I’d like to pick up on a key phrase from Dave’s story “My GP was happy to support the process but critically did not propose it.” What Dave is saying here is that this was a path to health not prescribed by his physician – instead he chose it himself, and that path less travelled made all the difference.
When a journey is optional to take, there is no prize for completing it and you track your progress along the way. When self-optimisation using data is wrapped in a digital medium such as a website or app, this is known as “success tracking” and it is growing in popularity.
The biggest advocates of the success tracking model are of course the makers of digital “fitness” pedometers such as those made by FitBit and its competitors. Indeed, this is already big business – Meticulous Research expects the worldwide success tracking for health market to grow to £2.8bn by 2022. So far so good, with many clinicians trialling a similar approach with their patients.
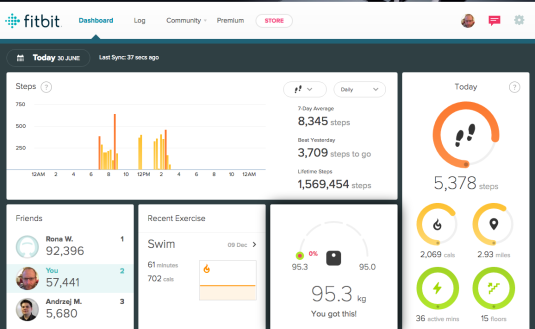
(Photo: fitbit dashboard by Toby Beresford)
However, it is all too easy for clinicians to ignore the design principles behind phenomenal growth of the activity trackers and default to the old-school “carrot and stick” model of motivation. They may expect to have the same take up with digital trackers for their disease area but by getting the motivational design wrong they may be surprised by their failure.
Daniel Pink, in his book Drive: the surprising truth about what drives us, calls the carrot and stick model “Motivation 2.0”. “If-then rewards” he says, “often do more harm than good.” It’s the next evolution of behavioural design, Motivation 3.0 that really works in the long term. Only when we give patients “Autonomy, Mastery and Purpose” will they truly succeed on their own.
Knowingly, or unknowingly, Dave Snowden’s “hero’s journey” used a classic Motivation 3.0 approach. He chose to ignore the palliative route for care expected of him and opted-in to a curative route. He tracked his own diet and exercise until he made a full recovery.
So, how can we replicate this new motivational model within the confines of our existing healthcare system and leverage the scale and affordability of a digital approach?
One key area to look at is preventative medicine. My next door neighbour, currently a few months shy of her 80th birthday, has recently joined a weekly “prediabetes” group after local screening highlighted her as being at risk. As well as attending training, she now tracks her cholesterol, weight, diet and exercise on a weekly basis. While not using a digital approach today, there is much in diabetes prevention that could be delivered more effectively and cost efficiently using a success tracking app.
It is in this sort of elective care that clinicians can most benefit from applying success tracking principles. There will be a huge difference in compliance when someone “owns” their journey as we tend to behave differently when we are measuring ourselves than when someone else measures us. For one, we are a lot more interested in the results.
As a regular swimmer I know this to be true in my own life. I now use a SwimTag at my local pool. It comes in the form of a bracelet, picked up at reception and worn during my swim. Later that day I always check the email notification to see how many lengths I managed. Sometimes I’ll drill down into the data to see how fast I swam and the stroke details within each length.
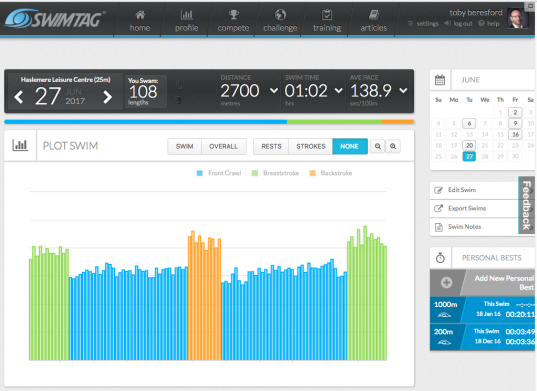
(Photo: SwimTag dashboard by Toby Beresford)
So, when it comes to health and digital disease management, patients who opt-in to take care of themselves are much more likely to achieve their goals than those who comply out of duty or subservience to authority.
How can we encourage patients to opt-in though?
Persuading patients to opt-in is of course the million dollar question. Clinicians vary in charisma and patients vary in their attitude and ability to comply!
While traditional persuasion techniques (ensuring full understanding, knowing the opportunities and risks, hearing stories from others who have travelled the same route, encouraging social support etc) will all be applicable, I’d like to focus on what we can do when designing the digital tools themselves. The medium is part of the message after all.
So, what should the tool do?:
Allow fast and granular opt-in and opt-out
I’d expect any tool to allow me to choose my privacy level. Maybe I could choose to appear on a benchmark ranking of other patients but appear as anonymous, or I could stay “unranked” but still see how I am performing against the average. Or, if I choose I could opt out all together. Few patients may choose this, but giving them the option to is critical to achieving buy-in. This level of privacy control is fundamental and implementing a patient success tracking program without it risks failure.
Connect to online social identities
I am much more engaged by results, scores and ranks put alongside my real name with my photo. If I’m comparing with others on the same journey then I’d like to see their current photo and name too. Facebook now has 2bn users, love it or hate it, integration with Facebook is de rigueur.
Feedback stories not just results
Human beings engage with stories more than they do with raw numbers. Data storytelling is a growing discipline and its principles should be used in any program. Telling someone they’ve hit a personal best this week is much more engaging than simply giving them their results and expecting them to work it out themselves.
Allow the magic of social proof to do its work
I’ve never forgotten my Psychology lectures with Solomon Asch. He showed that we will change our mind, even to the extent of declaring something patently false to be true, when confronted with a group of peers believing it. Conformity is a huge driver of behaviour change.
Provide easy ways to share progress back into social media
In his journey out of diabetes, Dave Snowden also talks about the value of his journey being made public, the fact that others were tuning in kept him on task. Now while a public figure like Snowden has many thousands of followers, there is no reason why this shouldn’t be true for every patient within their own social group. Sharing a health journey on social media may sound scary to Baby Boomers and Generation X but for Millennials it is close to being the norm.
What are the risks?
As with any new approach there are plenty of risks. Certainly any kind of behavioural approach, if designed badly, can have unwanted side effects. People respond to tracking programs in ways not easy to foresee when you are designing them.
One risk to be especially aware of is “gaming the system”. By ensuring there is no cash incentive or reward you cut out most of this (the only person a cheat cheats is themselves) but it is difficult to wipe out entirely. You could see patients focusing on one metric to an extreme degree – such as starving themselves to get their score (and weight) down.
Other unintended side-effects I’ve seen are where people take short cuts to achieve a higher score, clubbing together in cabals to beat the system. With people so focused on winning the “game” they are oblivious to what’s going on around them, even to the extent of breaking the law.
These issues are easy to identify but sometimes hard to prevent. That’s why following a good methodology can really help, or better still, getting motivational design help from an experienced “gamification” designer.
What are the opportunities?
But despite the risks, the opportunity for success tracking programs within health remains significant. Patients effectively treating themselves is a gold standard for public health – the closer to the patient you treat the disease the more cost effective it is. A hospital bed is an expensive way to care.
Success tracking apps can scale up and offer ways for patients to self-care, saving us all money.
Better health tracking can improve public health too. If we can avoid the development of more people with chronic diseases like diabetes the better it will be for society as a whole.
Trailblazed by FitBit, digital success tracking is at the beginning of what it can achieve in public health. I’m looking forward to seeing more programs developed over the next years – let’s just make sure everyone remembers to keep them opt-in!